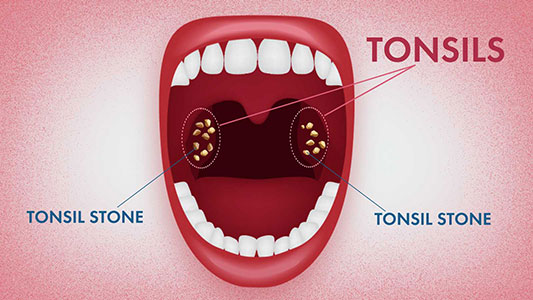
Tonsil stones, or tonsilloliths, are calcifications that form within the crevices of the tonsils.
When not calcified, these aggregations are known as chronic caseous tonsillitis (CCT). At St. Lawrence Dentistry, we frequently encounter these during our oral assessments. While the primary role of the tonsils is to trap inhaled pathogens, these structures are not without their complications. Tonsilloliths affect up to 10% of the population, often stemming from instances of tonsillitis.
How Do They Form?
These formations commonly emerge in older adults, with children being less prone. A prominent sign of their presence is bad breath. While usually asymptomatic, some may feel an odd sensation or as if something is lodged in the throat. Dr. Hawryluk notes that recurrent throat infections can escalate the incidence of these stones. They are comprised of biofilms teeming with various microbes. Although they mainly inhabit the palatine tonsils, they can also develop in the lingual tonsils. It’s not uncommon to discover large tonsil stones during medical or dental imaging conducted for other reasons.

Symptoms:
Often, tonsil stones might be symptomless, but they can be associated with foul breath, discomfort while swallowing, and a metallic taste. Other symptoms could include a sensation of the throat tightening, coughing, and gagging. Bigger tonsil stones might lead to persistent bad breath, earache, tonsil inflammation, and difficulty swallowing.
Treatment Approaches:
If tonsil stones aren’t causing discomfort, they might not need intervention. However, for those affected, remedies could range from swishing with salt water to employing chlorhexidine. However, for more severe or persistent cases, medical interventions, such as partial or complete removal of the tonsils, may be needed. We want to emphasize that while our office does help with gentle irrigating and cleaning around the tonsil area, we do not offer services like laser resurfacing, cryptolysis, or tonsil removal. For such advanced treatments or issues beyond the scope of dentistry, it’s imperative to consult a medical physician.

Home Remedies and Prevention:
Individuals may attempt to dislodge tonsil stones using clean cotton swabs. Oral irrigators can be beneficial, but one should exercise caution. Overly forceful irrigators might cause harm. It’s important to opt for tools that allow control over water pressure. At St. Lawrence Dentistry, we can provide guidance on suitable methods for your individual needs.

Moreover, swishing with lukewarm saline can help alleviate the pain of tonsillitis, which often accompanies tonsil stones.
While there are advanced procedures like laser cryptolysis that aim to prevent stone formation by smoothing the tonsil’s surface, remember that such procedures are not provided at our clinic. If you’re experiencing persistent issues with tonsil stones despite trying multiple remedies, it might be worth considering a consultation with a medical specialist.

Our Dedication to Oral Health Located in Mississauga, St. Lawrence Dentistry is committed to offering premier dental care. Although we’ve discussed tonsil stones in this article, our main focus remains on dental health. We thank you for trusting us with your care and for taking the time to read.
- Sleep Dentistry: Enhancing Comfort and Care During Dental Procedures - July 11, 2024
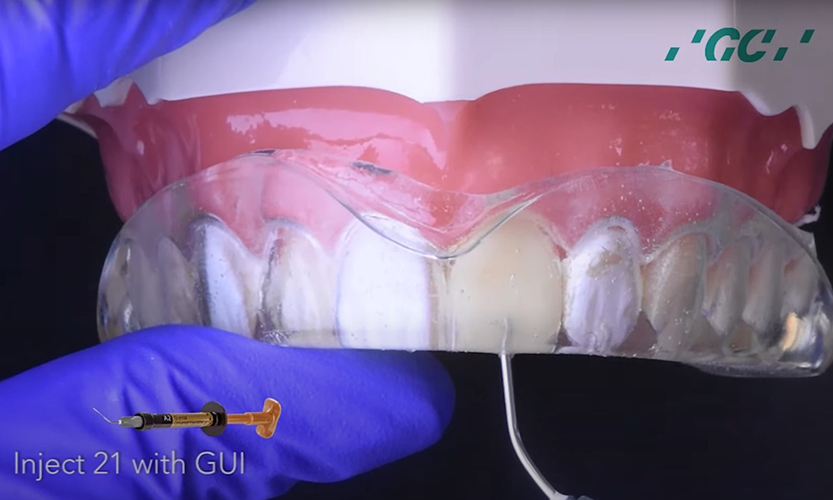
- The Revolutionary Injection Molding Technique for Composite Veneers - June 27, 2024
- Why Are Third Molars Called “Wisdom Teeth”? - June 19, 2024