One of St. Lawrence Dentistry chief goals is to remedy dental pain. This is an unpleasant feeling with physical and emotional components and it a very individual experience. It is usually caused by a tissue injury with elicits an emotional response. At the tissue level there is stimulation of a pain receptor. Pain receptors, also called nociceptors, are a group of sensory neurons with specialized nerve endings widely distributed in the skin, deep tissues (including the muscles and joints), and most of visceral organs.There is a whole variety of substances which will stimulate receptors and they are not unique in their jobs.
The substances that stimulate receptors are produced by the body during inflammation and have been called an ‘inflammatory soup’ which includes things like ‘vasoactive peptides’ (which alter blood vessel function), various kinins and mediators (including serotonin), adrenalin, bradykinin, and prostagladins. Each of these have specific receptors which are location specific. These are ubiquitous mediators which can be thought of as keys for different locks throughout the peripheral and central nervous system—when the doors open different things happen.
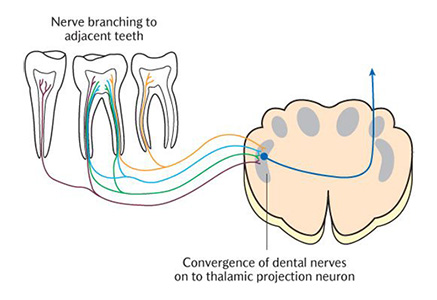
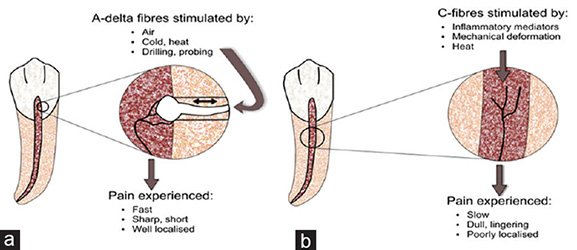
How do painful impulses get from your tooth to the brain? A pain stimulation travels through ‘A Delta and C fibers’. These are thinly or non-myelinated fibres which are very slow and very specific to transmitting obnoxious stimuli. They go through areas of the spinal nerve known as the ‘dorsal root ganglia’ and once they reach the central nervous system there are multiple relay stations which send the signal up into the brain. Multiple brain areas including the hippocampus, amygdala and prefrontal cortex are all involved with different aspects perceiving pain. The key feature here is there are multiple pathways and brain areas which makes pain management so difficult.
In dentistry we are primarily concerned with the oral facial regions and this area is primarily served by the ‘trigeminal nerve’ It has 3 divisions: ophthalmic (V1), maxillary (V2) and mandibular (V3). The nerve is mainly sensory but it does carry other types of branches. In the ophthalmic branch there are sympathetic nerves which control the aperture of the iris. (V2) is almost purely sensory and relays sensation from the sinus cavity, nasal wall, skin on face below the orbit, upper teeth, some of temple. (V3) is both sensory, motor, and parasympathetic. There are glandular functions in terms of salivary glands, skin sensation, teeth, muscles of mastication. It is big nerve and when it misbehaves a lot of interesting things can happen. If we look at (V2) there is a lot of air space in the sinus and nasal cavity that these nerves traverse. A lot of its branches follow the vasculature and they form neurovascular bundles that travel in groups. This is significant when we start taking about different tissues that can cause pain.
When we talk about types of pain we generally talk about the tissue the pain is associated with. One type pain is muscular pain. Acute muscular pain is usually triggered by a lack of oxygen getting to the muscles which leads to acidity buildup. This triggers sensory nerve endings which tells us the muscle hurts. In addition acute muscle pain is also caused by tears stretches and bruises. Chronic muscle pain is less understood. There are nodules in tender muscles and if you palpate them they will hurt. In fibromyalgia, a type of pain in irritated muscles, stimulating these nodules winds up activating ‘group 3 and 4’ nerve fibres which sends a message of pain to the brain.
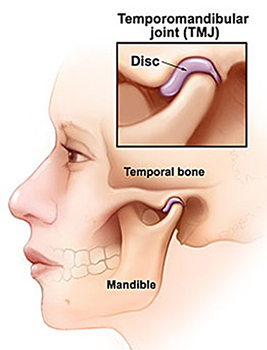
Skeletal pain is sometimes found in the dental joint (TMJ). It can be Inflammatory in nature and can be acute (trauma and infection) or chronic (degenerative and immunological). Chronic skeletal pain mostly affects joints. In addition, skeletal pain can be malignant in nature. The dental joint is very susceptible to wear and tear and this can cause little calcified centres to form which can impinge on soft tissue and cause pain. These tend to be chronic issues unless there is an acute injury.
Vascular pain relates to pain relating to blood vessels and can be very painful depending on the circumstance. The classic one is temporal arteritis which is inflammation of the temporal artery.
It is very graphic when it happens and can be mistaken for migraines because of the location. Trigeminal vascular pain is a tight blending of nerve and blood vessels. It is typically the basis for migraine pain. This can be difficult to deal with as it is recalcitrant and there are different receptors for this type of pain. Peripheral artery disease can cause vascular pain and is characterized by a poor circulation and metabolic changes to vessels. One of the worst vascular pains ever is ‘directing aneurisms’. This is when the walls of the vessels split and since they are so richly innervated. Finally another example of vascular pain is coronary artery disease. Heart attacks are painful for musculature and vascular reasons.
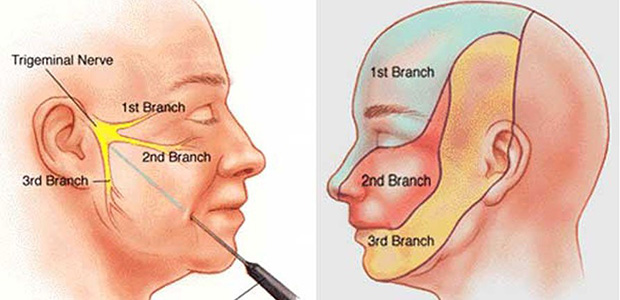
Another class of facial pain is nerve pain. This can be divided into the following subcategories: Neuritis—This is nerve inflammation and can be related to mechanic trauma . For example if an implant is placed near a nerve it can get inflamed. In addition, neuritis can be associated with viruses. Neuropathy—This is nerve degeneration and it is often the outer coating of the nerve or ‘myelin sheath’ which is the issue. Myelin is a lipid (fat) layer which creates electrical insulation and allow for the conduction of nerve impulses. Diabetes is one condition associated with neuropathies. Neuralgia is the last class of nerve pain and is unique in that there are no pathologic changes in nerve tissue. Often they can be transient but sometimes can linger for years. The most common dental neuralgia is ‘trigeminal neuralgia’ and is characterized by electric ‘lance like’ bouts of pain.
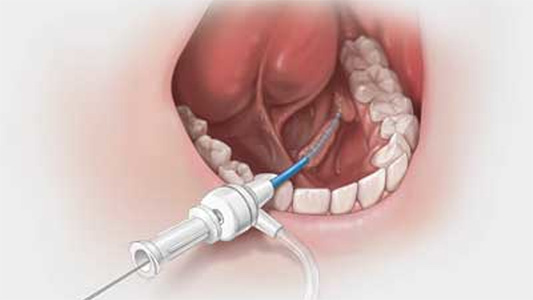
Pain of the glands is a category of pain that dentists have to diagnose. A gland is an organ in the human or animal body which secretes particular chemical substances for use in the body or for discharge into the surroundings. This pain is often related to an bacterial or viral infection which can cause obstructions in the gland. Inflammation can be a cause of glandular pain. For example, the parotid glands get can get blocked and saliva will build up. Stretching of tissue and pooling of saliva cause pain and it can become infected. The parotid gland is a major salivary gland. The two parotid glands are present on either side of the mouth and in front of both ears. They are the largest of the salivary glands. Autoimmune issues can cause gland pain and a notorious example is Sjogrens syndrome. This is a disorder of your immune system identified by its two most common symptoms — dry eyes and a dry mouth. Adenomas (benign gland tumors) or Neoplasms (cancerous growths) can also put pressure on glands creating glandular based pain. Sometimes tooth pain is actually originates from the sinus. The V2 branch of the trigeminal nerve runs in the sinus lining. If mucus builds up here it can put pressure on the nerve resulting in pain.
Mechanisms of acute and chronic pain are different and it is important that the dentist understand these so he/she is able to treat them appropriately. In acute pain free nerve endings are attached to nerve fibres called ‘C fibers’. These are unmyelinated slow transmission fibres. These are located among all kinds of other different fiber. Some of these are stretch, pressure, thermal fibres. All of these have different nerves leading up to the central nervous system. Free nerve endings are the only pain receptors. The other receptors are mostly mechanical but they will transmit pain when confronted with different stimuli. In other words, most nerve receptors have a primary job but its not their exclusive job. For example, a pressure receptors job is to inform of pressure, but if you exert too much pressure it will transmit pain. Different biochemical mediators will trigger these receptors in different ways so the transmission of pain is a complex subject.
Chronic pain is a little different from acute pain in that it involves ‘phenotypic switching’. This means nerves can change what they do depending on demand. In chronic pain the nerves that we are taking about are ‘interneurons’. These are in the spinal cord and exist as part of the ‘trigeminal nucleus’ (collection of nerve matter in the brain stem). They form part of the ‘reflex arc’ so when you are hurt the muscle pulls away so we don’t have to think about withdrawal. A reflex, or reflex action, is an involuntary and nearly instantaneous movement in response to a stimulus. A reflex is made possible by neural pathways called reflex arcs which can act on an impulse before that impulse reaches the brain. Interneurons are also ‘projection neurons’ which are nerve fibres which send up to the higher centres of the brain. This allows for signal interpretation.
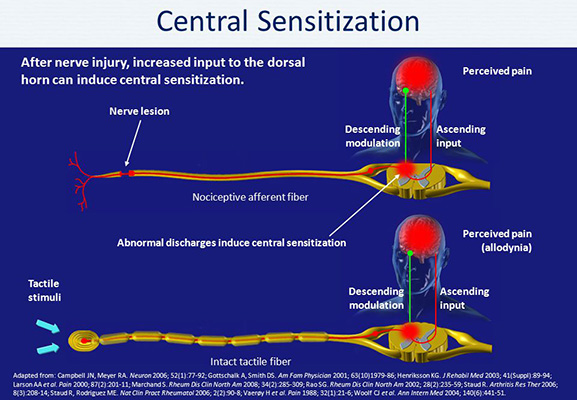
When pain changes from acute to chronic something interesting happens. The interneurons can ‘phenotypically switch’ to send stimuli to the higher brain areas. When this happens any stimulus whether it be temperature, pressure, can all come across as pain. This is the hallmark change in the transition from acute to chronic pain. The interneurons are phenotypically switched through a process called ‘genetic signalling’ which involves protein production at a cellular level.
After your nervous system has been receiving a pain signal for some time a process called ‘Central Sensitization’ can take place. It is characterized by more receptors in the pain sharing the receipt of the pain transmission. This in many cases means you can no longer define the specific area of discomfort, everything just hurts. This of course is one factor which makes chronic pain very difficult to treat.
One very fairly common type of pain seen in dentistry is ‘Phantom Pain’. This can happen when a sore tooth is taken out but the patient still feels like they have a sore tooth. The happens due to ongoing processing in the central nervous system even when stimuli is gone. In essence, the pain signal is getting bounced on the brain around and has a life of its own.
Although the biology of pain is complex, most dental discomfort can be easily treated at St. Lawrence Dentistry. In addition, we have a network of specialists we work with to help solve any dental issue you may be having. If you are looking for a dentist and live in the Mississauga area please give us a call.
Reference: University of Toronto, Faulty of Dentistry Lecture series, 2018.
- Sleep Dentistry: Enhancing Comfort and Care During Dental Procedures - July 11, 2024
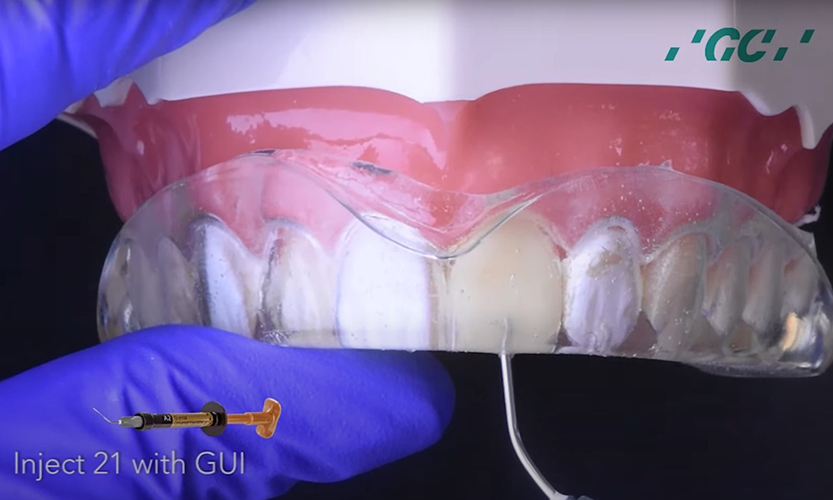
- The Revolutionary Injection Molding Technique for Composite Veneers - June 27, 2024
- Why Are Third Molars Called “Wisdom Teeth”? - June 19, 2024