St. Lawrence Dentistry recognizes the link between oral and total body health. In the last decade, there has been a concerted effort for the center for disease control to assess the prevalence of periodontal disease (gum disease) in the population.
About 67% of North American adults had some form of periodontitis (gum disease). Studies have shown the prevalence in Europe and Asia is comparable.
The biofilm (film of bacteria) in the mouth has biology quite different from those bacteria that were grown in single-cell planktonic culture, and they activate genes that promote antibiotic resistance. These bacteria can adhere firmly to the tooth surface and resist the flow of saliva and gingival fluid (liquid film in the gum tissue). The biofilm in periodontal disease is quite resistant to antibiotic therapy. They are 100-1000 times more resilient when compared to single cells, not part of a biofilm – this is why we cannot treat periodontal disease with antibiotics alone.
To learn more about Gum Disease and its treatment at our Mississauga Office, please visit us here:
Types Of Gingivitis
The human microbiome project has helped us understand oral organisms better. The goal was to identify and characterize microorganisms associated with healthy human beings. It has found that the human body contains about 10 trillion cells, but that bacteria residing in the body number about 100 trillion cells— hence they outnumber us 10 to 1.
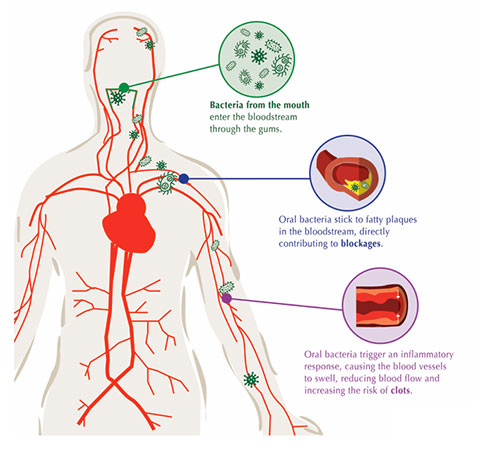
Ecological alterations cause periodontitis within the sub-gingival (below the gum line) microbiome. These organisms cause a local inflammatory response, which may cause periodontal tissue destruction. They also leak into the systemic circulation and create a low grade systemic inflammatory response. If you treat gum disease, these systemic bacteria will decrease. There is also the involvement of other types of organisms in gum disease — such as viruses, fungi, Protista.
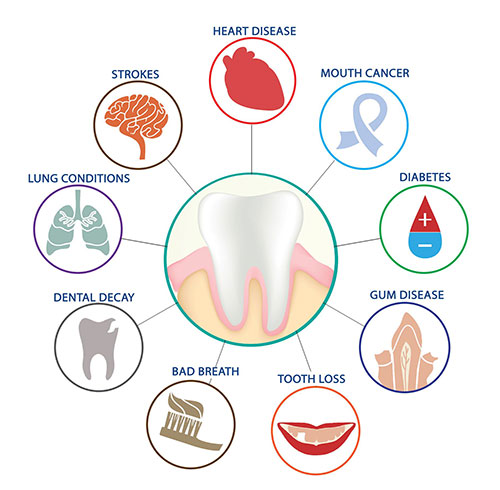
Systemic effects of periodontal disease include:
- Worsened glycemic control— increased complications in diabetes
- Increased risk of heart disease stroke and peripheral artery disease
- Increased respiratory illness in institutionalized patients
- Increased adverse pregnancy outcomes
- Increased cancer — oral and colon
The systemic inflammatory response is very damaging there are links to diabetes, heart disease, possibly cancer, and Alzheimer’s disease — a whole series of chronic disease which we don’t have an adequate explanation of their etiology. The relationship gives rise to the subject of inter-professional management of patients between physicians and dentists.
To read more about the link of Oral disease and Alzheimer’s disease please visit us here:
Is Alzheimers Disease Linked To Gum Disease?
Some people react more severely to a certain amount of plaque — this a due to host of risk factors. For example, if you are male, a smoker, older, or have diabetes, you are more at risk. Also, obesity, osteoporosis, low dietary calcium, stress are systemic risk factors.
Treatment for “systemic factors” involved in gum disease include:
- Co-management of diabetes
- Nicotine cessation
- Refined sugar restriction, weight management
- Reduction of rate of osteopenia (reduced bone mass) with a bone sparing agents
- Low dietary calcium
- Reduction of stress
There is a distinct body of evidence that suggests gum disease and diabetes potentiate off each other. The reason for this is periodontal infections contribute to insulin resistance. If you have diabetes, you will need to work with your physician to control your glycemic (sugar level) before and during your dental therapy. The worldwide incidence of diabetes 2000-2010 saw an incidence increase of 46 percent. The growth varies with the region, with Asia seeing the most at a 57% increase. The data is suggesting this increase is continuing from 2010 onwards is less in North America and Europe. However, still a significant increase in incidence. Many have called this an epidemic in type 2 diabetes. We have known for a long time there was a correction between diabetes and periodontal disease. Several studies have found there is a link between uncontrolled gum disease and the worsening of glycemic control. The good news is that dental therapy can interrupt the component of insulin resistance that is at least associated with periodontitis.
Diabetes is a systemic disease with the following complications:
- Increases risk of periodontal disease
- Leading cause of blindness in working adults (diabetic retinopathy)
- Leading cause of the end-stage renal disease (diabetic nephropathy)
- 2-4 fold increase in cardiovascular disease and stroke
- Leading cause of nontraumatic lower-extremity amputations (diabetic neuropathy)
There is also a profound relationship between gum disease and atherosclerosis. One study found there was a 72% greater risk for people having heart disease if they have periodontitis. (De Stefano et al. 1993) From people who had died from a stroke, it was found periodontal pathogens resided in these arteries, with a higher incidence compared to people who did not die of stroke (Genco and Fong 1998). There is evidence that something in the vessels signals the bacteria to congregate there. The gum bacteria ‘P.gingivalis’ can grow in the endothelial cells (cells lining vessels) of the heart. Periodontal bacteria likely act in concert with other factors such as hyperlipidemia, diabetes, hypertension, and smoking. It is not only from bacteria from the oral cavity but also bacteria from the gut and the skin— so this issue of cause is very multifactorial and complicated.
In summary, it appears that oral bacteria or the microbiome is mobile. It does transfer to other sites in the body where it can cause considerable damage. We know there are transient ‘bacteremias’ (rise in bacteria in the blood) whenever a patient with gums disease chews or flosses. Some of these bacteria go to the liver and react with proteins that cause systemic inflammation. Some bacteria go right to the heart and even to the placenta (the organ in uterus housing the fetus). There are even oral bacteria found in cancers. Heart disease and diabetes are among the leading causes of death in developed countries. Periodontal disease is also prevalent and related to both. Therefore prevention and treatment of periodontal disease and reducing common risk factors such as smoking and obesity contribute to overall health.
Dr. Hawryluk Jr. is a Mississauga Dentist who is committed to improving the oral health of his patients. If you would like to discuss this topic further, please call St. Lawrence Dentistry for an appointment.
References:
- Impact of Gum Disease on Overall Health: (2018) Reference Robert Genco Ph.D. Colgate Oral Health Network.
- De Stefano et al. 1993
- Genco and Fong 1998
- Sleep Dentistry: Enhancing Comfort and Care During Dental Procedures - July 11, 2024
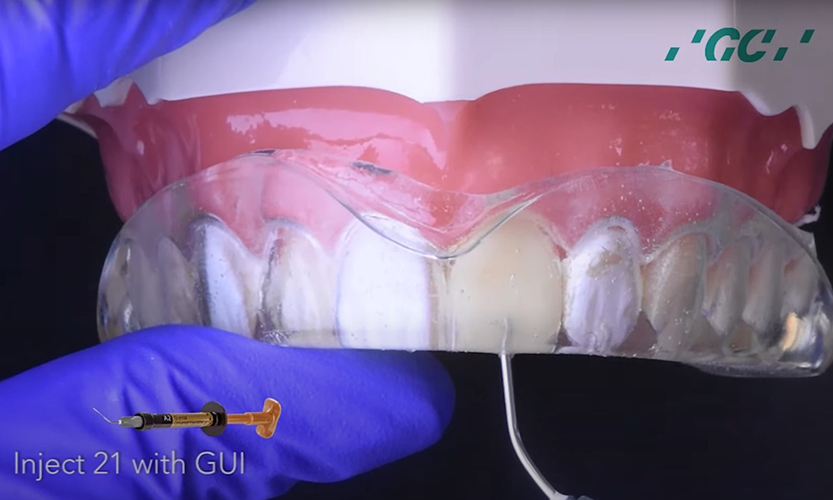
- The Revolutionary Injection Molding Technique for Composite Veneers - June 27, 2024
- Why Are Third Molars Called “Wisdom Teeth”? - June 19, 2024