St. Lawrence Dentistry recognizes the link between oral and total body health. Therefore, we make concerted efforts to treat periodontal disease (gum disease).
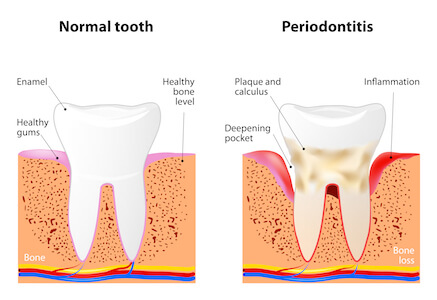
About 67% of North American adults have some form of periodontitis (gum disease). Studies have shown the prevalence in Europe, and Asia is comparable.
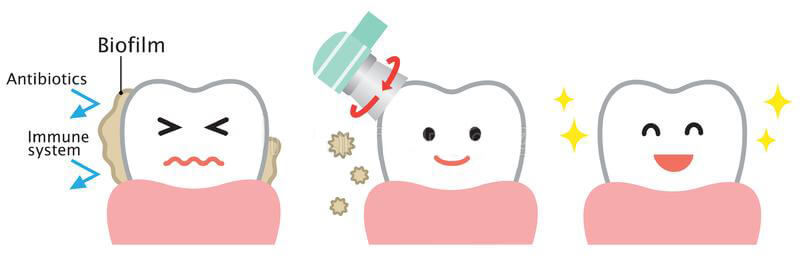
The biofilm (film of bacteria) in the mouth has biology quite different from those grown in single-cell planktonic culture, and they activate genes that promote antibiotic resistance. These bacteria can adhere firmly to the tooth surface and resist saliva and gingival fluid (liquid film in the gum tissue). As a result, the biofilm in periodontal disease is quite resistant to antibiotic therapy. They are 100-1000 times more resilient when compared to single cells, not part of a biofilm – this is why we cannot treat periodontal disease with antibiotics alone.
To learn more about Gum Disease and its treatment at our Mississauga Office, please visit us here:
The human microbiome project has helped us understand oral organisms better. Its goal was to identify and characterize microorganisms associated with healthy human beings. The human body contains about 10 trillion cells. The number of bacteria residing in our bodies is about 100 trillion cells. Hence the bacterial outnumber our cells 10 to 1. These organisms cause a local inflammatory response, which may cause periodontal tissue destruction. They also leak into the systemic circulation and create a low-grade systemic inflammatory response. If you treat gum disease, these systemic bacteria will decrease. There are also other types of organisms in gum disease that also have total body effects — such as viruses, fungi, Protista.
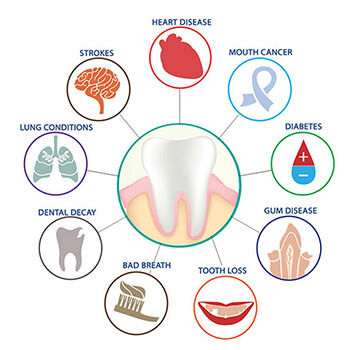
Systemic effects of periodontal disease include:
- Worsened glycemic control— increased complications in diabetes
- Increased risk of heart disease, stroke, and peripheral artery disease
- Increased respiratory illness in institutionalized patients
- Increased adverse pregnancy outcomes
- Increased cancer — oral and colon
The systemic inflammatory response of gum disease is very damaging. There are links to diabetes, heart disease, possibly cancer, and Alzheimer’s disease — a whole series of chronic diseases for which we don’t have an adequate explanation of their etiology. The relationship gives rise to the subject of inter-professional management of patients between physicians and dentists.

To read more about the link between oral disease and Alzheimer’s disease, please visit us here:
Is Alzheimer’s Disease Linked To Gum Disease?
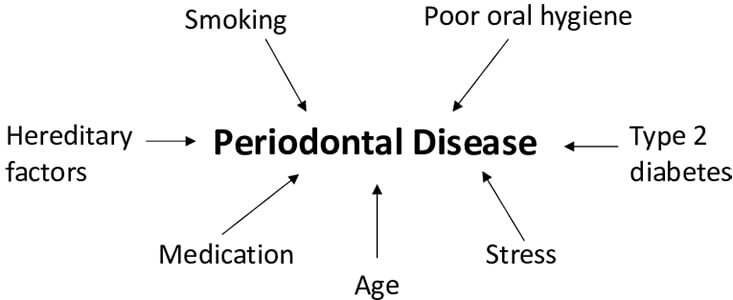
Some people react more severely to a certain amount of plaque due to a host of risk factors. For example, if you are male, a smoker, older, or have diabetes, you are more at risk. Also, obesity, osteoporosis, low dietary calcium, stress are systemic risk factors.
Treatment for “systemic factors” involved in gum disease include:
- Co-management of diabetes
- Nicotine cessation
- Refined sugar restriction, weight management
- Reduction of rate of osteopenia (reduced bone mass) with bone sparing agents
- Low dietary calcium
- Reduction of stress
There is a distinct body of evidence that suggests gum disease and diabetes potentiate off each other. The reason for this is periodontal infections contribute to insulin resistance. If you have diabetes, you will need to work with your physician to control your glycemic (sugar level) before and during your dental therapy. The worldwide incidence of diabetes between 2000-2010 saw an incidence increase of 46 percent. The growth varies with the region, with Asia seeing the most at a 57% increase. The data suggests this increase is continuing from 2010 onwards is more diminutive in North America and Europe. However, still a significant increase in incidence. Many have called this an epidemic in type 2 diabetes. We have known for a long time there was a correction between diabetes and periodontal disease. Several studies have found there is a link between uncontrolled gum disease and the worsening of glycemic control. The good news is that dental therapy can interrupt the component of insulin resistance that is at least associated with periodontitis.
Diabetes is a systemic disease with the following complications:
- Increases risk of periodontal disease
- Leading cause of blindness in working adults (diabetic retinopathy)
- Leading cause of end-stage renal disease (diabetic nephropathy)
- 2-4 fold increase in cardiovascular disease and stroke
- Leading cause of nontraumatic lower-extremity amputations (diabetic neuropathy)
There is also a profound relationship between gum disease and atherosclerosis. One study found a 72% greater risk for people having heart disease if they have periodontitis. (De Stefano et al. 1993) From people who had died from a stroke, periodontal pathogens resided in these arteries, with a higher incidence than people who did not die of stroke (Genco and Fong 1998). There is evidence that something in the vessels signals the bacteria to congregate there. The gum bacteria P.gingivalis can grow in the heart’s endothelial cells (cells lining vessels). Periodontal bacteria likely act in concert with other factors such as hyperlipidemia, diabetes, hypertension, and smoking. It is from bacteria from the oral cavity and bacteria from the gut and the skin, so this cause is very multifactorial and complicated.

In summary, it appears that oral bacteria or the microbiome is mobile. It does transfer to other sites in the body, where it can cause considerable damage. For example, we know there are transient bacteremia’s (rise in bacteria in the blood) whenever a patient with gums disease chews or flosses. Some of these bacteria go to the liver and react with proteins that cause systemic inflammation. Some bacteria go right to the heart and even into the placenta (the organ housing the fetus). There are even oral bacteria found in cancers. Heart disease and diabetes are among the leading causes of death in developed countries. Periodontal disease is also prevalent and related to both. Therefore, prevention and treatment of periodontal disease and reducing common risk factors such as smoking, and obesity contribute to overall health.
Dr. Hawryluk Jr. is a Mississauga Dentist who is committed to improving the oral health of his patients. If you would like to discuss this topic further, please call St. Lawrence Dentistry for an appointment.
References:
Impact of Gum Disease on Overall Health: (2018) Reference Robert Genco Ph.D. Colgate Oral Health Network.
De Stefano et al. 1993
Genco and Fong 1998
- Unraveling the Enigma of Tooth Resorption - April 24, 2024
- Detecting Oral Cancer Early: The Importance of Regular Screenings - April 7, 2024
- The Ultimate Guide to Dental Hygiene: Tips for a Healthy Smile - March 31, 2024